Cirrhosis of the Liver Overview
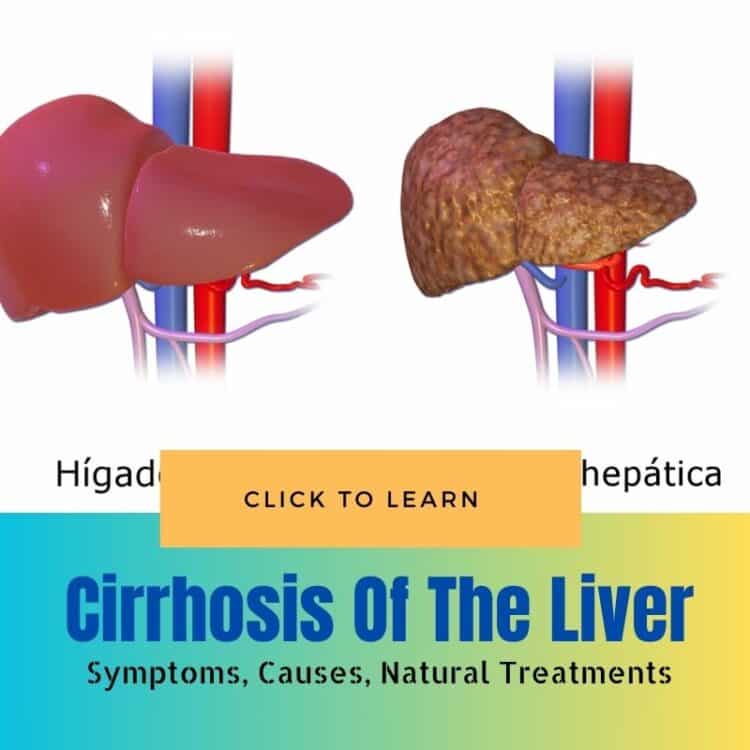
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions such as hepatitis and chronic alcoholism. Each time the liver is injured, it tries to repair itself. In the process, scar tissue forms. As the cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function.
Symptoms of Cirrhosis
The symptoms of cirrhosis can be quite varied ranging from mild to severe depending on the extent of liver damage. Among the common symptoms are fatigue, easy bruising, jaundice (yellowing of the skin), itchy skin, swelling in the legs and abdomen and weight loss.
Causes of Cirrhosis
Cirrhosis is most often caused by long-term exposure to toxins such as alcohol or viral infections. Chronic alcohol abuse, hepatitis B, hepatitis C and fatty liver disease are prominent factors that might lead to the development of cirrhosis.
Treatment Options for Cirrhosis
Treatment for cirrhosis depends on the cause and extent of liver damage. Approaches may include medication, lifestyle changes such as alcohol abstinence and weight loss and in severe cases, a liver transplant may be necessary.
Diet Recommendations for Cirrhosis
People with cirrhosis are often advised to follow a high-calorie, protein-rich diet to combat malnutrition. Reducing salt intake is also critical to help manage swelling in the body.
What Is Cirrhosis of the Liver Overview
Cirrhosis of the liver is a chronic and progressive condition in which the liver slowly deteriorates and is unable to function normally due to chronic long-term damage. This gradual degradation leads to scarring of the liver tissue also known as fibrosis which progresses to cirrhosis when significant. The extensive scarring interrupts the blood flow through the liver and impairs its ability to process nutrients hormones medications and toxins. Cirrhosis also disrupts the production of proteins and other substances made by the liver.
Definition of Cirrhosis of the Liver
Cirrhosis is defined as a late stage of scarring (fibrosis) of the liver caused by various forms of liver diseases and conditions such as hepatitis and chronic alcoholism. The liver carries out several necessary functions including detoxifying harmful substances in your body aiding in digestion and converting food into energy. When cirrhosis occurs tissue in the liver becomes fibrotic and the structure and function of the liver are irreversibly altered if the underlying causes are not addressed adequately and promptly.
Symptoms of Cirrhosis Early Signs to Watch For
Fatigue and Weakness – Fatigue is one of the most common early signs of cirrhosis. Individuals may experience a profound sense of tiredness that is not relieved by rest. This occurs because the liver is unable to efficiently process toxins and nutrients which in turns affects overall energy levels.
Poor Appetite – Loss of appetite is frequently reported among those with early-stage cirrhosis. This symptom can be attributed to changes in metabolism and digestive issues as the liver function declines.
Weight Loss – Unintentional weight loss often accompanies the loss of appetite. As the liver struggles to metabolize and store nutrients effectively, patients may start to lose weight without intending to.
Abdominal Pain and Bloating – Pain or discomfort in the upper right quadrant of the abdomen is a telltale sign of liver stress or damage. Bloating can also occur due to fluid buildup as the diseased liver struggles to regulate fluids properly.
Swollen Ankles and Legs – Edema or swelling in the lower extremities can occur due to increased pressure in the blood vessels around the liver and reduced protein production. This makes it difficult for the body to retain fluid in the blood vessels, thus causing it to accumulate in the tissues of the legs and ankles.
Easy Bruising and Bleeding – As cirrhosis progresses, it interferes with the liver’s ability to produce proteins necessary for blood clotting, leading to an increased tendency to bruise or bleed easily.
Changes in Skin Color – Jaundice, characterized by a yellowing of the skin and eyes results from the liver’s diminished capacity to process bilirubin. Moreover, certain skin changes like spider angiomata (small, spider-like capillaries visible under the skin) may also appear as an indicator of cirrhosis.
Itchy Skin – Accumulation of bile salts under the skin can cause persistent itching, which is often more severe during the night.
Confusion and Poor Concentration – A build-up of toxins in the bloodstream that are usually broken down and removed by the liver can affect brain function, leading to issues such as confusion or difficulty concentrating known as hepatic encephalopathy.
Common Causes of Liver Cirrhosis
Chronic Alcohol Consumption is a primary cause of liver cirrhosis. It leads to alcoholic liver disease where repetitive damage and inflammation occur due to excessive alcohol intake. Over time this causes scar tissue to replace healthy liver tissue.
Hepatitis B and C are viral infections that can lead to liver cirrhosis. Both viruses cause liver inflammation and long-term, continuous inflammation can result in extensive scarring, reducing the liver’s ability to function efficiently.
Nonalcoholic Fatty Liver Disease (NAFLD) including nonalcoholic steatohepatitis (NASH) occurs due to the accumulation of fat in liver cells in individuals who consume little or no alcohol. It often progresses to cirrhosis especially in the presence of obesity and diabetes.
Autoimmune Hepatitis entails the body’s immune system attacking the liver causing chronic inflammation and ultimately scarring. This autoimmune disorder can progress to cirrhosis.
Biliary Cirrhosis resulting from diseases such as Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC) can lead to cirrhosis. These diseases gradually destroy the bile ducts in the liver causing harmful substances to build up and scar liver tissue.
Genetic Disorders such as Wilson’s disease and Hemochromatosis directly impact the liver’s function by causing excessive buildup of copper and iron respectively in the liver leading to cirrhosis.
Risk Factors of Liver Cirrhosis
Alcohol Abuse significantly increases the risk of developing cirrhosis. Regular heavy drinking over a period of years subjects the liver to repeated tissue injury leading to cirrhosis.
Chronic Viral Hepatitis especially hepatitis B and C are significant risk factors as they persistently inflame the liver over years thereby enhancing the risk of cirrhosis.
Obesity is linked closely with NAFLD which increases the risk of developing cirrhosis. Excessive body weight often contributes to fat deposition in the liver thereby making it prone to inflammation and scarring.
Diabetes increases the risk of cirrhosis particularly among those with NAFLD as the high blood sugar levels associated with diabetes tend to exacerbate liver inflammation and fibrosis.
Age can be a factor because the risk of liver cirrhosis increases as the liver processes years of dietary and environmental toxins. Older individuals might have a higher risk due to prolonged exposure to these risk factors.
Treatment and Management of Cirrhosis
Treatment for cirrhosis is aimed at stopping or delaying the disease progression treating the complications and reducing the risk of liver cancer.
Lifestyle Changes
Avoiding alcohol – Complete abstinence is crucial as alcohol accelerates liver damage even in those with non-alcoholic related cirrhosis.
Eating a healthy diet – A balanced diet rich in fruits vegetables and whole grains can help manage cirrhosis. Limiting salt intake is also essential to prevent fluid buildup in the body.
Regular exercise – Maintaining a healthy weight through exercise can help prevent fat accumulation in the liver which can further exacerbate the condition.
Medications
Water pills (diuretics) – These help remove excess fluid and prevent swelling in the legs and abdomen.
Beta blockers or nitrates – Used to lower blood pressure in the veins that supply the liver (portal hypertension) which can reduce the risk of bleeding from varices.
Antibiotics – To prevent or treat infections patients might be prescribed antibiotics especially if they have developed ascites.
Procedures and Surgery
Endoscopic treatments for varices – If there are swollen blood vessels (varices) they may be treated with banding procedures to reduce the risk of bleeding.
Paracentesis – Removing fluid from the abdomen when it becomes uncomfortable or affects breathing.
Liver transplant – In severe cases or when the liver fails a transplant may be necessary. Liver transplant involves replacing the diseased liver with a healthy one from a donor.
Management of Complications
Monitoring and treatment of Hepatic encephalopathy – Medications like lactulose may be used to help reduce toxins in the blood which are normally cleared by the liver.
Screening for liver cancer – Regular screening for liver cancer by ultrasound with or without a blood test for alpha-fetoprotein may be advised based on the stage of cirrhosis and other risk factors.
Future and Experimental Treatments
Research is ongoing in the following areas to improve cirrhosis treatment Liver dialysis – A technique to help filter toxins from the blood mimicking the liver’s functions. Gene therapy and stem cell therapy – These are prospective treatments aimed at regenerating damaged liver cells or replacing the diseased liver tissue with healthy tissue.
Dietary Changes to Support Liver Health with Cirrhosis
Making the right dietary choices is crucial in managing cirrhosis and supporting liver health. Here are some essential nutritional guidelines to follow.
Reduce Sodium Intake
Eating less sodium is key to preventing fluid buildup in the body, a common issue in cirrhosis. Avoid adding salt to food when cooking or eating, and steer clear of high-sodium products such as canned foods, processed snacks, and ready meals. Opt for fresh fruits and vegetables, and prepare meals from scratch to better control your sodium intake.
Increase Protein Consumption
Protein is essential, but it should be consumed in a manner that the liver can handle. Focus on lean sources of protein such as poultry, fish, eggs, and dairy products. Plant-based proteins like beans, legumes, and tofu are also beneficial. Consult with a healthcare provider to determine the right amount of protein for your condition, as protein needs can vary based on liver function.
Limit Fatty Foods
Reducing intake of saturated fats and trans fats is crucial for liver health. Choose monounsaturated and polyunsaturated fats found in olive oil, nuts, and fish. Baking or grilling food rather than frying helps reduce unnecessary fat consumption.
Choose High-Fiber Foods
Dietary fiber aids digestion and can help improve the overall function of the liver. Include a variety of fiber-rich foods such as whole grains, fruits, vegetables, and legumes in your diet. Fiber not only helps with digestion but also regulates blood sugar levels and can aid in lowering cholesterol.
Avoid Alcohol
Consuming alcohol can significantly worsen liver damage. Abstaining from alcohol is vital to prevent further liver deterioration and complications in cirrhosis. If avoiding alcohol is challenging, seek professional help or support groups specialized in alcohol cessation.
Control Calorie Intake
Managing calorie intake is essential to avoid unhealthy weight gain or loss. Eating balanced meals and controlling portion sizes can help maintain a healthy weight. Due to the potential for muscle wasting in cirrhosis, monitoring caloric intake to ensure sufficient energy levels throughout the day is beneficial.
Stay Hydrated
Proper hydration is vital, especially for those with cirrhosis. Drink adequate amounts of water throughout the day to help flush toxins from your body and maintain kidney function. However, if there are restrictions on fluid intake due to your cirrhosis, be sure to follow your healthcare provider’s recommendations closely.
Consider Vitamin and Mineral Supplements
Cirrhosis can interfere with the body’s ability to process certain vitamins and minerals. It might be necessary to take supplements, especially for vitamins A, D, E, and K; however, it should always be done under the guidance of a healthcare professional to avoid complications such as toxicity or further liver strain.
Seek Professional Dietary Advice
It is advisable to consult a registered dietitian who understands cirrhosis to create a personalized meal plan. Dietary needs can vary greatly from person to person, especially concerning liver health and cirrhosis. A professional can tailor dietary recommendations to best support your liver function and overall health.
Conclusion
Cirrhosis of the liver represents a severe stage of liver disease characterized by extensive scarring of liver tissue which impairs its ability to function properly. Major causes include chronic alcohol consumption, hepatitis infections, and fatty liver disease. Symptoms are often silent in the early stages but may eventually include jaundice, fatigue, and abdominal swelling.
Effective treatment focuses on managing the symptoms and slowing the progression of the disease. This may include medications to control liver damage, procedures to manage complications, and in severe cases, a liver transplant. Lifestyle changes are critical, with a diet low in sodium and rich in fruits and vegetables being beneficial. Avoiding alcohol and managing associated conditions like diabetes and obesity can also prevent further liver damage.
Ultimately timely recognition and treatment along with sustained lifestyle adjustments offer the best outcomes for those suffering from cirrhosis.